Confirmation
Download PDF
Open All
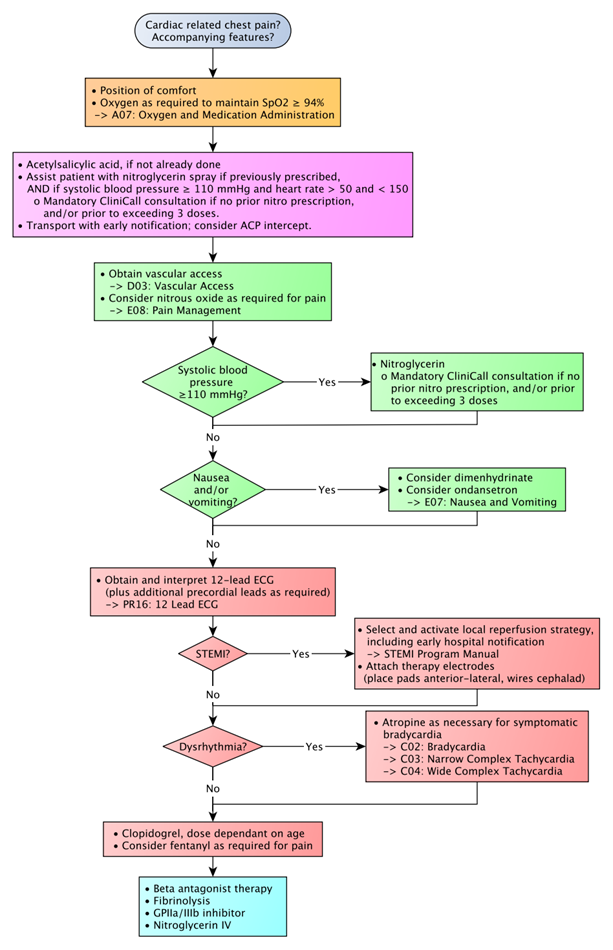
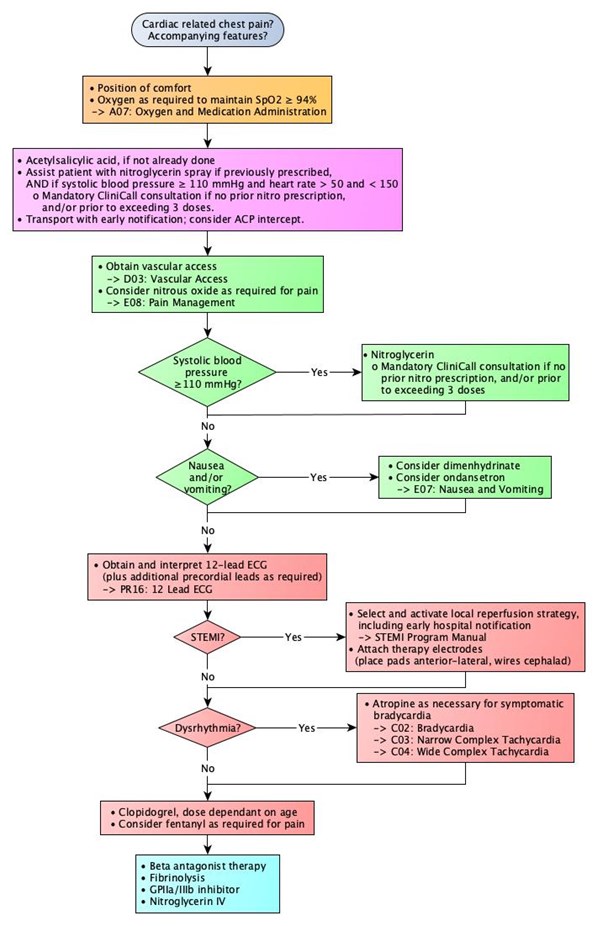
C01: Acute Coronary Syndrome
Updated:
Reviewed:
Introduction
The acute coronary syndromes represent a spectrum of diseases resulting from insufficient blood flow through the coronary arteries, with a wide range of presentations.
Essentials
- Rapid identification of STEMI to facilitate timely reperfusion strategies is the primary goal of prehospital management. Consider ACP intercept for ECG acquisition and interpretation if not available at the scene.
- Antiplatelet therapy should be initiated as early as possible in all patients with suspected coronary ischemia
- Reduction of myocardial oxygen demand should be accomplished wherever and whenever possible (i.e., management of nausea, pain, and limiting patient exertion)
Additional Treatment Information
- Acetylsalicylic acid (ASA) is the prehospital antiplatelet drug of choice. Emergency medical dispatch will instruct patients to chew and swallow ASA 320 mg, and patients may have taken their own prior to paramedic arrival. Unless otherwise contraindicated, ASA should be administered to bring the total dose, for this event, to at least 160 mg orally.
- Nitroglycerin, 0.4 mg sublingually, may be given to alleviate pain in cases of angina. Systolic blood pressure must be monitored prior to and during nitroglycerin therapy. Nitroglycerin has not been demonstrated to change outcomes in ischemic chest pain, and may in fact worsen myocardial ischemia under some circumstances. The on-going use of nitroglycerin in patients who have not experienced symptom relief following the first few doses is unlikely to produce any benefit.
- To minimize handover delays in suspected STEMI and to facilitate angiography and fluoroscopy, place therapy electrodes anterolaterally, with wires positioned cephalad prior to initiating transport.
- Vascular access: All patients with suspected coronary ischemia should have vascular access established with running intravenous fluid. When selecting a site for access, use of the distal third of the right arm is relatively discouraged (particularly in the setting of anticipated percutaneous coronary intervention). Do not delay transport to obtain vascular access.
General Information
- ACS exists on a spectrum, from angina through to STEMI:
- Angina is pain resulting from a temporary increase in myocardial oxygen demand. This may be the result of reduced blood flow in the coronary arteries as a result of arterial narrowing, or spasm in the arterial wall.
- Non-ST elevation MI (NSTEMI) is the result of an incomplete occlusion of a coronary artery, either by a thrombus alone or in concert with vasospasm. ECGs generally show ST segment depression or T wave inversion; transient ST segment elevation may also be observed.
- ST elevation MI (STEMI) occurs when a coronary artery is completely occluded by thrombus. The diagnosis is dependent on ST segment elevation in two or more anatomically contiguous leads.
- Classic presentations include chest pain, pressure, or discomfort associated with shortness of breath, nausea, and/or diaphoresis. Be aware that although these are common findings, certain populations – in particular, women, the elderly, those with a history of diabetes, and younger individuals – may present differently. Atypical ACS presentations can include weakness or fatigue, syncope/presyncope, abdominal pain, and nausea.
- The presence of palpable chest wall pain does not exclude ischemic origins. Paramedics should maintain a high suspicion of ischemic-origin pain in cases of chest pain without a clear history of trauma.
- Patients presenting with symptoms consistent with ACS should be managed as such regardless of ECG findings, up to and including transport destination selections.
- Contraindications to acetylsalicylic acid therapy include known allergy or hypersensitivity, or a recent history of upper or lower gastrointestinal bleeding. Patients on oral anticoagulant therapies are often told by their physician to avoid ASA. In the setting of suspected or known ACS, the antiplatelet activity of ASA is of more importance than the temporary rise in INR. Consult with CliniCall if unsure.
Interventions
First Responder (FR) Interventions
- Supplemental oxygen as required
Emergency Medical Responder (EMR) & All License Levels Interventions
- Oxygen as required to maintain SpO2 ≥ 94%
- Acetylsalicylic acid chew and swallow, if not already done
- Assist patient with nitroglycerin spray if systolic blood pressure ≥ 110 mmHg and heart rate > 50 and < 150
- Mandatory CliniCall consultation (1-833-829-4099) if no prior nitro prescription, and/or prior to exceeding 3 doses.
- Position of comfort
- Transport with early notification; consider ACP intercept
Primary Care Paramedic (PCP) Interventions
- Obtain vascular access with running intravenous fluid
- Nitroglycerin spray, every 4-5 minutes if systolic blood pressure ≥ 110 mmHg.
- Mandatory CliniCall consultation (1-833-829-4099) if no prior nitro prescription, and/or prior to exceeding 3 doses.
- Consider dimenhyDRINATE for nausea
- Consider nitrous oxide as required for pain
- If trained and authorized:
- Obtain and transmit 12-lead ECG
- If STEMI criteria are met:
- Obtain physician consultation prior to transport destination selection to verify treatment plan and selection of reperfusion strategy
- Attach therapy electrodes (place pads anterior-lateral, wires cephalad)
- → STEMI Program Manual
Advanced Care Paramedic (ACP) Interventions
- Obtain and interpret 12-lead ECG (plus additional precordial leads as required)
- In cases of STEMI:
- Select and activate local reperfusion strategy, including early hospital notification
- → STEMI Program Manual
- Consider eligibility for out-of-hospital reperfusion pathways.
- Select and activate local reperfusion strategy, including early hospital notification
- Attach therapy electrodes (place pads anterior-lateral, wires cephalad)
- Consider fentaNYL as required for pain
- Manage dysrhythmias as necessary
- Atropine as necessary for symptomatic bradycardia
- → C03: Narrow Complex Tachycardia
- → C04: Wide Complex Tachycardia
Critical Care Paramedic (CCP) Interventions
- Ticagrelor
- Heparin / low molecular weight heparin
- Nitroglycerin IV
- Fibrinolysis in consultation with EPOS/cardiologist
Algorithm
Evidence Based Practice
References
- Kawakami S, et al. Time to reperfusion in ST-segment elevation myocardial infarction patients with vs. without pre-hospital mobile telemedicine 12-lead electrocardiogram transmission. 2016. [Link]
- Welsford M, et al. Part 5: Acute coronary syndromes: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. 2015. [Link]