Confirmation
Download PDF
Open All
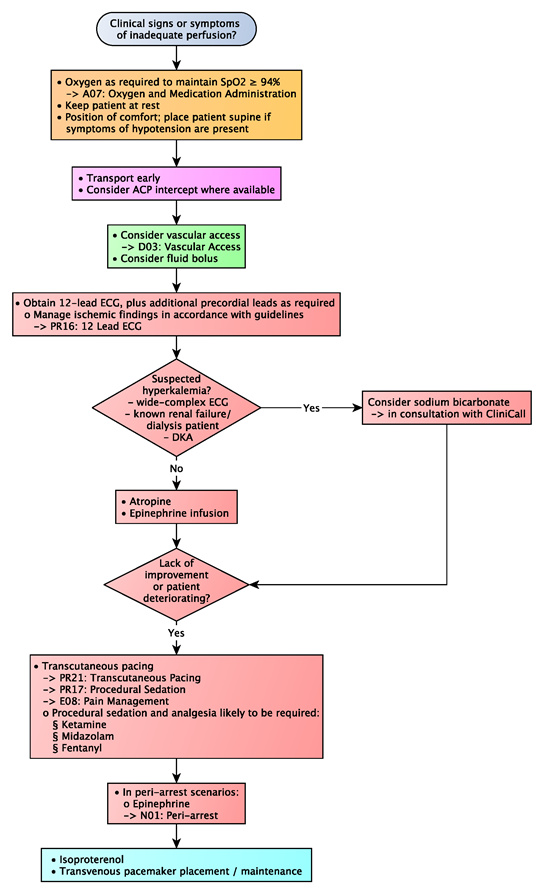
C02: Bradycardia
Updated:
Reviewed:
Introduction
While bradycardia is defined as a heart rate of less than 50 beats/minute, symptomatic bradycardia refers to weakness, a decreased level of consciousness, shortness of breath, hypotension, or chest pain that is the result of bradycardia. The treatment of bradycardia focuses on optimizing hemodynamics and addressing the underlying cause.
Essentials
- Patients with bradycardia often complain of dizziness, which is frequently exacerbated by positional changes and resolves when positioned supine, or mild shortness of breath. These patients can be managed with supportive care only, provided they are otherwise asymptomatic.
- Patients with adequate perfusion and a low heart rate may require monitoring and transport, but no treatment. Unless the patient requires immediate resuscitation, a conservative approach to management should prevail.
- Clinical end points are defined by the amelioration of symptoms rather than any particular heart rate or blood pressure.
- Management of the prevailing underlying condition is often more critical than correction of the dysrhythmia.
Additional Treatment Information
- Although atropine remains the first-line therapy in adult symptomatic bradycardia, it is unlikely to be effective in 2nd and 3rd degree heart blocks; its use is, however, still recommended in these cases. Atropine is ineffective and potentially harmful in patients who have had a heart transplant.
- Small doses of atropine may produce a transient slowing of the heart rate. In these cases, administer a second dose immediately. In long transports, additional atropine may be required to sustain its effect to a maximum total dose of 3 mg.
- Epinephrine infusion should be considered in cases where atropine has failed to produce a meaningful improvement in heart rate or blood pressure.
- Rapid intervention in patients who are peri-arrest (i.e., who have a markedly decreased level of consciousness and signs of profound hypoperfusion) can prevent further deterioration and stave off a progression to cardiac arrest. Epinephrine, rather than atropine, is the preferred treatment option in these cases, but note that there is no published data that supports the routine use of epinephrine in preference to atropine for patients not at imminent risk of cardiac arrest.
- Renal failure can precipitate hyperkalemia, which can in turn cause a dangerous accumulation of AV node blocking agents (calcium channel or beta blockers), producing significant bradycardia and hypoperfusion (the so-called BRASH syndrome). This is often triggered by underlying hypovolemia in elderly patients with pre-existing renal dyfunction. Fluid resuscitation and consultation with CliniCall for management of suspected hyperkalemia are recommended.
General Information
- In all cases of bradycardia, consideration must be given to the overall clinical condition of the patient. Signs of effective perfusion (particularly skin color and temperature, and mentation) are better indicators of the need for intervention than blood pressure (either systolic blood pressure or mean arterial pressure) alone. Paramedics should have a nuanced understanding of the degree to which a patient is symptomatic.
- In all cases of symptomatic bradycardia, search for and address treatable or reversible causes. Such cases may include:
- Hypoxia (especially in younger patients)
- Increased parasympathetic (vagal) tone
- Drug effects or overdoses
- Hyperkalemia, with or without concurrent metabolic acidosis
- Myocardial ischemia, particularly if it involves the SA or AV nodes and conduction system
- In the setting of myocardial infarction, bradycardia is often compensatory and somewhat beneficial. Be cautious of initiating rate-specific therapies as these may increase myocardial oxygen demand and extend the margins of infarct. Therapy should be reserved for those patients who are significantly hypotensive.
Interventions
First Responder (FR) Interventions
- Supplemental oxygen as required
- Keep patient at rest
- Position of comfort; place patient supine if symptoms of hypotension are present
Emergency Medical Responder (EMR) & All License Levels Interventions
- Oxygen as required to maintain SpO2 ≥ 94%
- Transport early
- Consider ACP intercept where available
Primary Care Paramedic (PCP) Interventions
- Consider vascular access
- Consider fluid bolus
Advanced Care Paramedic (ACP) Interventions
- Obtain 12-lead ECG, plus additional precordial leads as required
- Manage ischemic findings in accordance with guidelines
- Consider sodium bicarbonate only in cases of suspected hyperkalemia (wide-complex ECG, known renal failure/dialysis patient, diabetic ketoacidosis), in consultation with CliniCall.
- Atropine to effect
- EPINEPHrine infusion to effect (increase dose q 2-3 minutes)
- Transcutaneous pacing
- In peri-arrest scenarios:
- Consider push-dose EPINEPHrine
- → N01: Peri-arrest
Critical Care Paramedic (CCP) Interventions
- Isoproterenol
- Transvenous pacemaker placement / maintenance
Algorithm