Confirmation
Download PDF
Open All
PR09: Continuous Positive Airway Pressure
Applicable To
Introduction
Continuous positive airway pressure (CPAP) devices provide a non-invasive method of improving oxygenation in patients who are experiencing significant respiratory distress. The use of CPAP eases work of breathing, supports alveolar recruitment, decreases overall mortality, and reduces the need for intubation.
Indications
Patients who are:
- Awake and able to follow commands
- Able to maintain an open airway
- Over 13 years of age
- Exhibiting respiratory distress with all of the following:
- Respiratory rate > 24/minute
- SpO2 < 94% on supplemental oxygen
- Use of accessory muscles
- Consider the use of CPAP in adult patients with respiratory distress, including but not limited to:
- Congestive heart failure or acute cardiogenic pulmonary edema
- Asthma
- Submersion injuries
- Pneumonia
- Chronic obstructive pulmonary disease
Contraindications
- Patients less than 13 years old
- Decreased level of consciousness, or inability to follow commands
- Respiratory arrest or hypoventilation
- Patients who are in imminent or actual respiratory failure (i.e., whose respirations are slow, feature shallow tidal volumes, and whose level of consciousness is falling) are not candidates for CPAP. These patients must be ventilated with a bag-valve mask (and may benefit from PEEP use).
- Unable to fit mask to patient’s face
- Vomiting or any other risk of aspiration
- Traumatic cause of respiratory distress
- Tracheostomy
- Suspected or known pneumothorax
- Systolic blood pressure < 90 mmHg
Procedure
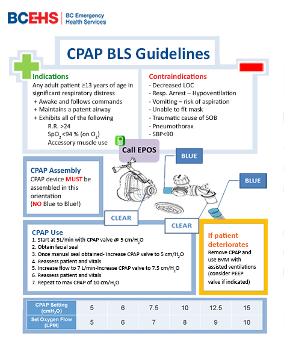
Primary care paramedics must consult with CliniCall (1-833-829-4099) prior to starting CPAP therapy
- Assemble appropriate equipment. Verify mask sizing by comparing the mask to the patient’s face.
- Explain the procedure and obtain consent.
- Position the patient in an upright, sitting position. Attach pulse oximeter.
- Connect the CPAP mask to the oxygen source. Set the flow to 5 LPM if possible (otherwise use 6 LPM).
- Have the patient hold the CPAP mask over their nose and mouth. A progressive application of pressure to obtain a seal may be required to maximize the acceptance of the mask. Paramedics should be calm and reassuring.
- Once the patient appears to be able to tolerate the mask, position the bonnet over the back of the head and attach the straps to the side of the mask. Adjust the Velcro and headpiece for optimal seal.
- Examine the mask seal for leaks. Reassess the patient.
- If SpO2 remains below 92%, follow the manufacturer’s flow rate chart. Incrementally raise the oxygen flow to increase both FiO2 and CPAP pressure. Do not exceed 10 cmH2O.
Notes
- Do not attempt to use the CPAP mask for bag-valve ventilations.
- Oxygen saturations may transiently fall during initial CPAP use. Allow time for the mask to work before adjusting the therapy.
- Do not delay the administration of medications to apply a CPAP mask.
- Use conventional therapies (e.g., bronchodilators) first in patients with audible wheezing. Nebulizers, connected to the mask with a T-piece, may be attached to the auxiliary port on the CPAP mask; in this case, increase the oxygen flow rate by 7-8 LPM.
- A do-not-resuscitate order or MOST does not preclude the use of CPAP for relief from shortness of breath.
Resources
References
- BLS Systems. Rescuer II Compact CPAP System. [Link]