Confirmation
A03: Clinical Handover & Communication
Updated:
Reviewed:
Introduction
Clinical handover of a patient represents a vulnerable time during patient care. The WHOs Joint Commission report of 2014 on Sentinel Event Data identified ineffective communication during handover as one of the most common root causes for sentinel events. Sentinel events are defined as any unanticipated event in a healthcare setting resulting in death or serious physical or psychological injury to a patient or patients, not related to the natural course of the patient's illness. In addition, the WHO World Alliance for Patient Safety has identified improvements in communication during patient handovers as a key factor in improving patient safety.
The WHO has presented two guiding principles to minimize communication errors and/or omissions during clinical handover. First, the handover should be tailored to the discipline that it is being used in with context given to end users of the information. Second, the contents of the handover should be standardized in the order that they are presented. By standardizing the contents of a clinical handover it will create a shared mental model between the sender and receiver and convey all necessary clinical information.
Essentials
- Key principles for effective clinical handover include:
- Appropriate environment for handover should protect patient confidentiality and limit non-critical interruptions during handover.
- Clinical handover information should be timely, accurate and devoid of repetition. Use of common language and minimal use of abbreviations recommended.
- Handovers should be structured consistently to guide the content and flow of information in a manner that suits the clinical context and contain a minimum standard of information.
- The purpose of a standardized clinical handover process is to ensure the safe, effective and structured exchange of information during handover of ambulance patients in the emergency department or receiving facility. Studies have noted that verbal clinical handovers are prone to inaccuracies and omissions; whereas documentation of verbal reports are also subject to frequent error.
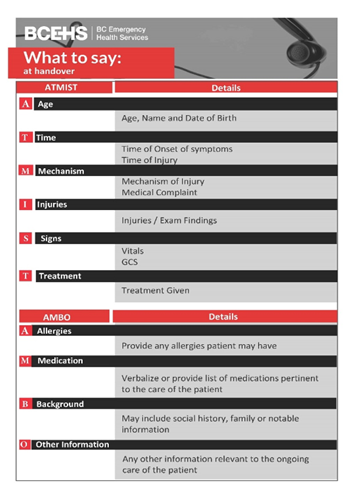
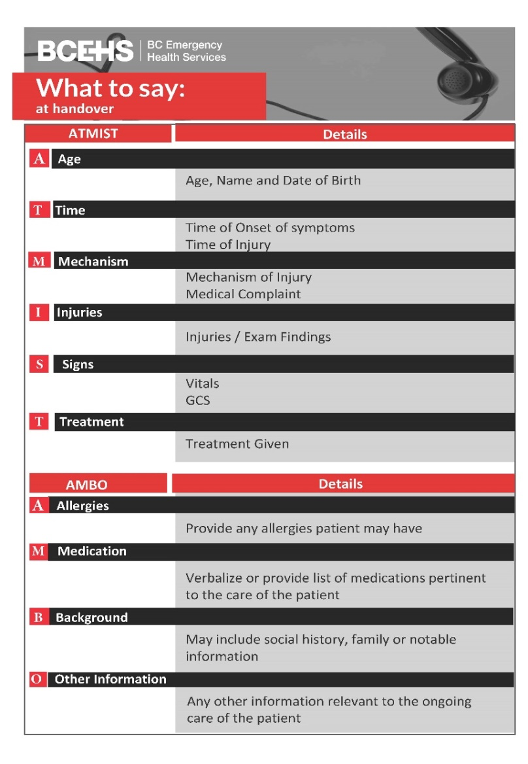
- ATMIST AMBO is a standardized handover model that adheres to WHO guiding principles as mentioned above.Research suggests that implementing standardized clinical handovers reduces adverse events and communication related errors in patient care. The use of acronyms and mnemonics is useful to help structure the contents of a clinical handover as they facilitate rapid information recall.
- Clinical handover of a critical patient should include a 20-30 second period where the patient remains on the ambulance stretcher with a “hands-off, eyes on” period until the ATMIST information is delivered (excluding critical interventions).
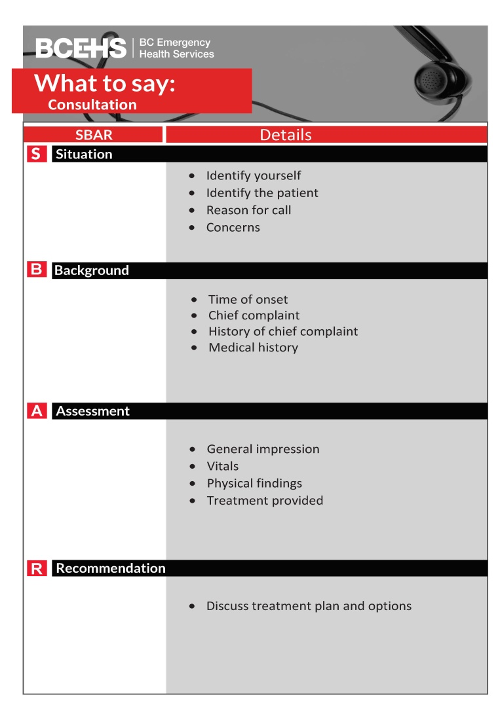
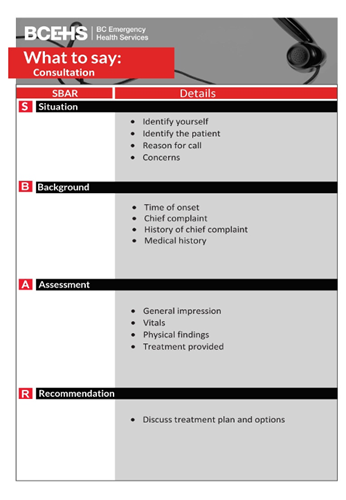
- SBAR: Provides an easy to use structured form of communication that enables information to be transferred accurately between individuals. Effective tool for use during telephone consultation with EPOS/CliniCall. SBAR helps to reduce communication barriers between different levels of staff and provides clarity of expectations for both the sender and receiver of information.
Interventions
Emergency Medical Responder (EMR) & All License Levels Interventions
References
- Arora V, et al. Patient Handoffs. In UpToDate. 2020. [Link]
- Bates DW, et al. Global priorities for patient safety research. 2009. [Link]
- Bost N, et al. Clinical handover of patients arriving by ambulance to the emergency department - a literature review. 2010. [Link]
- Carter AJE, et al. Information loss in emergency medical services handover of trauma patients. 2009. [Link]
- Dawson S, et al. Review article: Improving the hospital clinical handover between paramedics and emergency department staff in the deteriorating patient. 2013. [Link]
- Evans SM, et al. Assessing clinical handover between paramedics and the trauma team. 2010. [Link]
- Evans SM, et al. Clinical handover in the trauma setting: A qualitative study of paramedics and trauma team members. 2010. [Link]
- Foster S, et al. The effects of patient handoff characteristics on subsequent care: A systematic review and areas for future research. 2012. [Link]
- Goldberg SA, et al. Quantitative analysis of the content of ems handoff of critically ill and injured patients to the emergency department. 2017. [Link]
- Iedema R, et al. Design and trial of a new ambulance-to-emergency department handover protocol: 'IMIST-AMBO'. 2012. [Link]
- Jensen SM, et al. Handover of patients: A topical review of ambulance crew to emergency department handover. 2013. [Link]
- Joint Commission. Sentinel Event Data: Root causes by event type 2004-2014. 2014. [Link]
- Logarajah S, et al. An integrated ABCDE approach to managing medical emergencies using CRM principles. 2014. [Link]
- Meisel ZF, et al. Optimizing the patient handoff between emergency medical services and the emergency department. 2015. [Link]
- Murray SL, et al. Quality of the handover of patient care: A comparison of pre-hospital and emergency department notes. 2012. [Link]
- Owen C, et al. Lost in translation: Maximizing handover effectiveness between paramedics and receiving staff in the emergency department. 2009. [Link]
- Sanjuan-Quiles A, et al. Handovers of patients from prehospital emergency services to emergency departments. 2018. [Link]
- Shah Y, et al. Clinical handover between paramedics and emergency department staff: SBAR and IMIST-AMBO acronyms. 2016. [Link]
- WHO Collaborating Centre on Patient Safety Solutions. Communication during patient hand-overs: Patient safety solutions. 2007. [Link]
- Wood K, et al. Clinical handovers between prehospital and hospital staff: Literature review. 2015. [Link]
- Yong G, et al. Handover from paramedics: Observations and emergency department clinician perceptions. 2008. [Link]