Confirmation
L02: Normal Labour and Delivery
Updated:
Reviewed:
Introduction
In the prehospital realm, childbirth is defined as the unplanned delivery of a newborn outside of a hospital, which may or may not require resuscitation. “Imminent delivery” is defined as the moment when the head, buttocks, or legs, of the baby become visible at the vaginal opening between contractions. This is also known as crowning, and signals that delivery will occur within minutes.
Childbirth is a natural process, and only a small number of cases will require aggressive intervention. The successful transition from intrauterine to extrauterine life depends on significant physiological changes that occur at birth, and although most newborns make this transition successfully, a small but significant number will require additional support, including resuscitation; paramedics must, therefore, prepare for the case where acute care and intervention are required. It is critical to remember that maternity cases involve at least two patients, and both require assessment.
Essentials
- Labour consists of 3 stages:
- 1st stage: Dilation of cervix by regular and painful contractions. This stage may last up to 12 hours.
- 2nd stage: Birth of the infant. This stage may last between 2 and 3 hours, but can also be much shorter in subsequent deliveries.
- 3rd stage: Delivery of the placenta. This stage may last up to 1 hour.
- Signs of imminent and inevitable delivery include the following:
- Delivery imminent when contractions are less than 2 minutes apart and very strong.
- Delivery is inevitable if the perineum is bulging, the head is crowning or the patient complains of an urge to “push”, “bear down”, or “have a bowel movement”.
- Uncomplicated/normal birth:
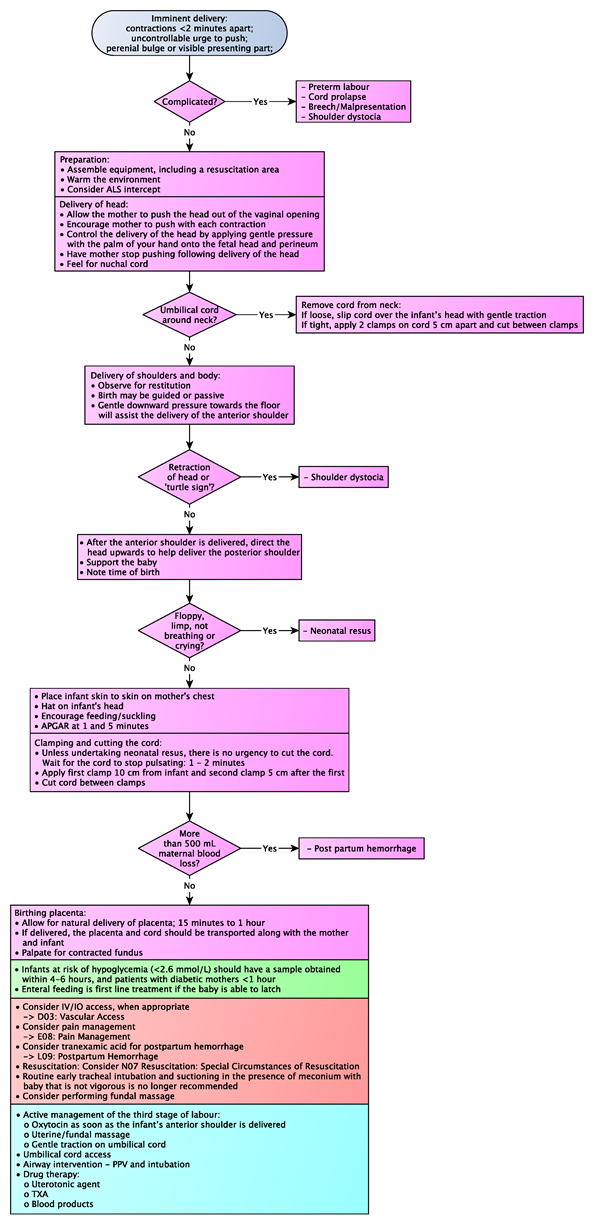
- See Adult Childbirth - Imminent Delivery Algorithm in Additional Treatment section
- The uncomplicated delivery
- Term gestation with breathing and crying infant with good tone
- Infant stays with mother, skin to skin, continued observation and maintain warmth
- Complicated/high risk birth:
- → L08: Complications of Delivery (malpresentation, shoulder dystocia, cord prolapse)
- → L07: Preterm Labour
- → L09: Postpartum Hemorrhage
- Multiples: Ensure that sufficient resources are assigned to each patient. Note that multiples (twins, triplets, etc) often deliver early. Review CPG L07: Preterm Labour for additional information.
- Cord clamping: It is now accepted and preferred practice to delay cord clamping at least 30 to 60 seconds, or longer. The practice is appropriate for healthy vigorous infants without birth complications. If resuscitation is required, the cord should be clamped immediately to facilitate the care of the neonate.
- In the event that neonatal resuscitation is required, follow the NRP principles
Additional Treatment Information
- Patient assessment considerations
- Consider known malpresentation of fetus (e.g., breech, shoulder dystocia).
- Consider seeking consultation and additional resources as necessary
- Provide supplemental oxygen as required to maintain SpO2 ≥ 94%
- Consider establishing IV access if further treatment is required
- General principles for managing the delivery of the child:
- Delivery should be controlled so as to allow a slow controlled delivery of the infant
- Support the infant’s head as needed
- Check the umbilical cord around the neck. If it is present, slip it over the head. If unable to free the cord from the neck, double clamp the cord and cut between the clamps.
- Grasping the head with hands over the ears, gently pull down to allow delivery of the anterior shoulder
- Gently pull up on the head to allow delivery of the posterior shoulder
- Slowly deliver the remainder of the infant
- Clamp the cord 2 inches from the abdomen with 2 clamps and cut the cord between the clamps
- Calculate and record APGAR scores at 1 and 5 minutes
- Refer to NRP guidelines for neonatal assessment and resuscitation. See CPG M09: Neonatal Resuscitation for additional details.
- General principles for care of the mother:
- The placenta will deliver spontaneously, usually within 5 minutes of the infant. Do not force the placenta to deliver.
- Massaging the fundus may decrease bleeding by facilitating uterine contractions after delivery of the placenta
- Consider tranexamic acid in uncontrolled vaginal bleeding
- Consider manual in utero pressure and packing
- Consider nitrous oxide for pain control. Narcotics should be reserved as a last resort
- Midwives may give oxytocin or misoprostol for uncontrolled post-partum bleeding due to uterine atony
Referral Information
- All patients in labour should be transported to the nearest hospital unless delivery is imminent, or the patient’s primary care provider (i.e., midwife) is advising otherwise.
- Patients under the care of a midwife may refuse transportation to a hospital following a delivery. This is a discussion to have with all parties present with a goal of family centered decisions and care.
General Information
- The APGAR score is the tool most commonly used to assess neonates. The APGAR should be performed at 1 and 5 minutes of life.
|
Strength and regularity of heart rate |
|
|
100 beats/minute or more (2 points) |
|
|
Less than 100 (1 point) |
|
|
None (0 points) |
|
|
Lung maturity |
|
|
Regular breathing (2 points) |
|
|
Irregular (1 point) |
|
|
None (0 points) |
|
|
Muscle tone and movement |
|
|
Active (2 points) |
|
|
Moderate (1 point) |
|
|
Limp (0 points) |
|
|
Skin colour/oxygenation |
|
|
Pink (2 points) |
|
|
Bluish extremities (1 point) |
|
|
Totally blue (0 points) |
|
|
Reflex response to irritable stimuli |
|
|
Crying (2 points) |
|
|
Whimpering (1 point) |
|
|
Silence (0 points) |
|
Interventions
Emergency Medical Responder (EMR) & All License Levels Interventions
- If the decision is made to deliver in the field:
- Assemble equipment, including a resuscitation area
- Warm the environment, including towels and blankets if able. This should result in the room or space being uncomfortably warm.
- Position the mother:
- Supine
- Sims (lateral with knees to chest)
- Alternate: will vary based on situation
- Delivery of the infant (second stage):
- Allow the mother to push the head out of the vaginal opening - note that paramedics are not trained to do internal vaginal exams to determine if the patient is fully dilated and effaced.
- Control the delivery of the head by applying gentle pressure with the palm of your hand onto the fetal head and perineum. Feel for nuchal cord.
- If present, gently lift it over the infant’s head. DO NOT pull hard on the cord as avulsion can occur, gentle traction is acceptable. Clamping and cutting the cord may be necessary if it cannot be reduced. Delivery must be completed quickly if the cord is cut.
- Support the baby’s head and guide the delivery of the shoulders. Gentle downward pressure towards the floor will assist the delivery of the anterior shoulder. After the anterior shoulder is delivered, direct the head upwards to help deliver the posterior shoulder.
- If shoulder dystocia is suspected, see →L08: Complications of Delivery
Post-delivery care of the infant:
- Once the infant is delivered: clear mouth then nose of secretions if grossly contaminated, dry, stimulate and reposition while ensuring warmth is maintained. Place the infant on the mother’s chest (+/- polyethylene bag).
- Routine suctioning of the mouth and nose is no longer recommended.
- If necessary, a 6 Fr catheter can be used. Suction should be turned down to less than 100 mmHg.
- The use of food grade polyethylene plastic bags to place the newborn in has become an effective method to prevent hypothermia in both term and preterm neonates. Cover the newborn up to the shoulders and do not secure the bag in any way around the neck. Place a hat on the newborn’s head and transport in a warm ambulance with the ambient temperature at 22 to 26 degrees Celsius.
- Cord clamping:
- Should be delayed at least 30 to 60 seconds in term and preterm vigorous infants. Place the clamps approximately 4 cm apart from each other and cut in between.
- Assess the infant:
- APGAR at 1 and 5 minutes of life (see APGAR in General Information section)
- Normal vital signs for a newborn:
- Temperature target is between 36.1°C and 37°C axillary
- Heart rate - 120-160 beats per minute (can be felt at the base of the umbilical cord or by auscultation)
- Respiratory rate - 35-60 breaths per minute (should be counted over a full minute)
- SpO2: Target pre-ductal (right hand) SpO2 after birth:
- 1 minute: 60-65%
- 2 minutes: 65-70%
- 3 minutes: 70-75%
- 4 minutes: 75-80%
- 5 minutes: 80-85%
- 10 minutes: 85-95%
- Blood pressure can be measured using a neonatal-size blood pressure cuff in infants with suspected cardiovascular or renal abnormalities, but is rarely performed on low risk infants.
- Blood glucose level - in healthy term newborns, routine blood glucose screening is not indicated
- Delivery of the placenta (third stage):
- The placenta should naturally deliver on its own within 30 minutes. Manipulation is often not required. Once delivered, the placenta and cord should be transported along with mother and infant.
- Up to 500 mL of blood loss from mother is normal with childbirth. Anything in excess of that amount, refer to L09 Postpartum hemorrhage
Primary Care Paramedic (PCP) Interventions
- Infants at risk of hypoglycemia (<2.6 mmol/L) should have a sample obtained within 4-6 hours, and patients with diabetic mothers <1 hour.
- Enteral feeding is first line treatment if the baby is able to latch
Advanced Care Paramedic (ACP) Interventions
- Consider IV/IO access, when appropriate
- Consider pain management
- Consider tranexamic acid for postpartum hemorrhage
- Routine early tracheal intubation and suctioning in the presence of meconium with baby that is not vigorous is no longer recommended
- Consider performing fundal massage
Critical Care Paramedic (CCP) Interventions
- Active management of the third stage of labour:
- Oxytocin as soon as the infant’s anterior shoulder is delivered
- Uterine/fundal massage
- Gentle traction on umbilical cord
- Umbilical cord access
- Airway intervention
- Drug therapy:
- Uterotonic agent
- TXA
- Blood products
Algorithm