Confirmation
Download PDF
Open All
E04: Dialysis Emergencies
Updated:
Reviewed:
Introduction
Patients who suffer from an acute or chronic injury or illnesses to their kidneys are at risk of developing kidney failure. Treatment options depend upon the patient’s clinical condition and comorbidities, and range from conservative treatment with medication and fluids, to peritoneal dialysis or hemodialysis, to kidney transplantation.
Essentials
- Patients requiring renal dialysis often have numerous other medical problems, including hypertension, diabetes, and cardiovascular disease. Paramedics should be alert to the possibility of concurrent clinical issues.
- Do not attempt to take blood pressures, or start an intravenous, in an extremity that has a dialysis shunt or fistula in place.
- Always consider the possibility of hyperkalemia in patients on dialysis or with renal failure.
- Dialysis patients should be transported preferentially to a facility capable of providing dialysis services. If the patient is critically ill, transport the patient to the nearest facility. Contact CliniCall for assistance with destination choices.
Referral Information
It may be reasonable to bypass the emergency department in favor of transport to the patient’s dialysis clinic. Consult with CliniCall is encouraged.
General Information
- Peritoneal dialysis uses the peritoneal membrane in the body itself as a filter. This membrane is a fine layer of tissue lining the peritoneal cavity. The peritoneal cavity’s rich vascular supply makes the peritoneal membrane ideal for filtering metabolic wastes and excess fluid from the blood. Dialysis solution is instilled into the abdominal cavity via a surgically inserted Tenckhoff Catheter. Metabolic waste products then pass from the bloodstream, across the peritoneal membranes, and into the dialysis solution. After a period of dwelling time, the solution is drained from the peritoneal space and replaced with a fresh solution.
- In hemodialysis, blood is pumped from the body through special tubing into a dialysis machine from a surgically inserted catheter or arterio-venous (AV) fistula. This typically occurs 3 or 4 days per week at a dialysis center, but can also be performed daily at home. The hemodialysis machine removes waste products and excess fluid from the blood and, as such, acts as a type of artificial kidney. The blood passes through a dialyser (filter), which also assists in balancing fluids and electrolytes in the blood. The machine then returns the filtered and cleansed blood to the body at the same rate at which it is removed.
- Patients undergoing hemodialysis will have a long-term catheter or shunt placed for this procedure. Catheters are typically placed in the upper chest groin, and shunts are typically placed in the arms or forearms. The shunt is created by anastomosing a vein and an artery; a thrill can be felt on the shunt when it is palpated, and a bruit can be heard when it is functioning properly.
- Common complications of dialysis treatment include:
- Infection at the shunt or catheter site, or systemically
- Direct fingertip pressure with gauze should be performed at the site of the bleeding
- Disequilibrium syndrome develops when a shift of metabolic waste and electrolytes occurs, causing weakness, dizziness, nausea and / or vomiting and seizures
- Hypotension can cause altered LOC, angina, seizures, or arrhythmia, and typically responds to small fluid bolus of 250 mL normal saline
- Occlusion or disruption of the Tenckhoff catheter
- Some medications are filtered out by the dialyser, limiting their therapeutic effect
- Air embolism
- Shunt bleeding typically following a hemodialysis session, and will occur in 1 to 4 tiny holes made by needles. Apply direct pressure to control. When the bleeding stops tape over the gauze, but do not remove the gauze to check for control as this will usually cause more bleeding. Circumferential dressings, if used, should not be used as this can occlude the shunt and cause clotting. The tape should, at a maximum, envelope about 180 degrees of the extremity.
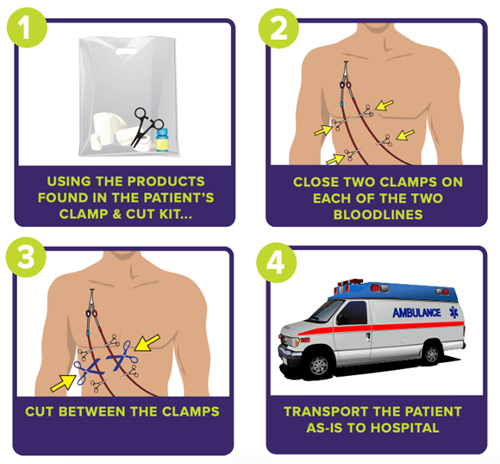
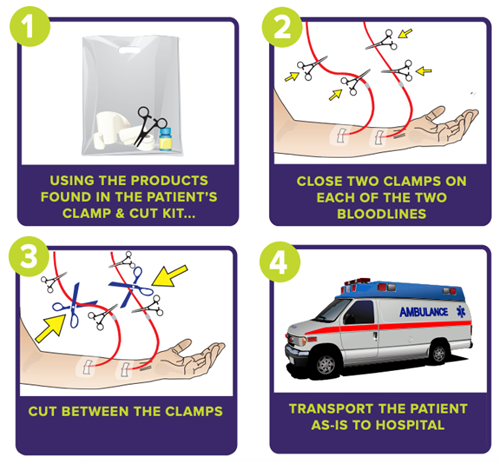
Emergency Disconnect Instructions
For dialysis patients with a central catheter:
For patients with a fistula or graft:
Interventions
First Responder (FR) Interventions
- Keep patient at rest
- Control bleeding as required
- Position patient based on comfort and prevent heat loss
Emergency Medical Responder (EMR) & All License Levels Interventions
- Transport in position of comfort
- Perform emergency disconnect from home dialysis machine if patient is critically ill
Primary Care Paramedic (PCP) Interventions
- Obtain vascular access.
- → D03: Vascular Access
- Normal saline if systolic blood pressure is < 90 mmHg, or if signs of end-organ hypoperfusion exist.
- Correct hypoglycemia:
Advanced Care Paramedic (ACP) Interventions
- In patients with significant hemodynamic instability or dysrhythmia, and a suspicion of hyperkalemia: