Confirmation
Download PDF
Open All
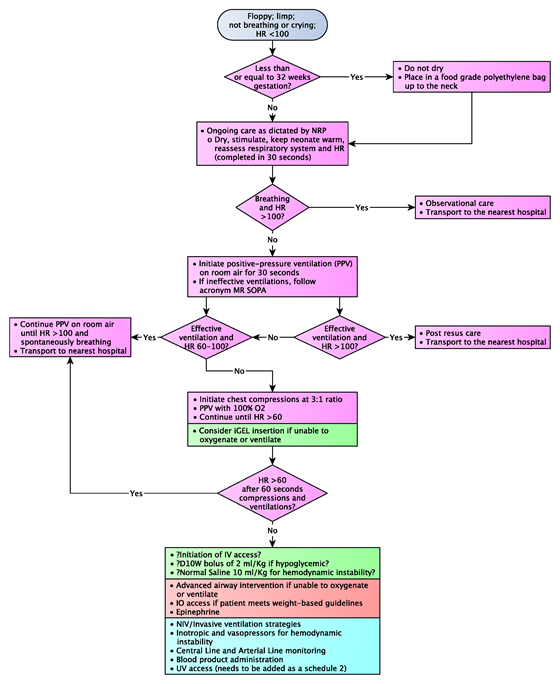
M09: Neonatal Resuscitation
Updated:
Reviewed:
Introduction
Neonatal resuscitation focuses on the respiratory system and transitioning from fetal circulation to neonatal circulation. These two factors are interrelated; a functioning respiratory system is necessary to deliver oxygen to produce pulmonary vasodilation, thus lowering the pulmonary vascular resistance. When combined with increasing systemic vascular resistance, this allows fetal shunts to close and lung perfusion to progress.
Paramedic management in the resuscitation of the neonate focuses on stabilizing the respiratory system in a systemic manner from least invasive to most invasive.
Essentials
- The Neonatal Resuscitation Program (NRP) has a clearly defined algorithm for all neonatal resuscitation events. Each step in the algorithm requires 30 seconds of effective intervention prior to moving on to the next step.
- During the first 30 seconds, begin by assessing the neonate’s tone. Are they term, breathing or crying?
- Tone: a neonate should be active with flexed extremities. If the neonate is flaccid with extended extremities resuscitation will be required.
- Term: if the neonate is less than 37 weeks gestation, they require an initial assessment as they are more likely to require assistance either immediately or soon after delivery.
- Breathing or crying: a strong cry is a sign of a strong respiratory system. If the neonate is not crying, then a respiratory assessment for work of breathing is required and possible movement down the resuscitation chart.
- In the next 30 seconds, dry, stimulate, keep the neonate warm, and reassess the respiratory system and take a heart rate.
- Following the first minute, a decision is required: does the neonate require respiratory support (blow by oxygen, CPAP) or respiratory assistance (positive pressure ventilation - PPV)?
- If the patient requires PPV then 30 seconds of effective ventilation is initiated. Effective ventilation is described as adequate chest expansion with all breaths. If all breaths are not effective, then the acronym MR SOPA should be reviewed:
- M – Mask: Is there adequate seal
- R – Reposition: reposition the head, consider shoulder roll.
- S – Suction: use a 10 fr suction catheter and suction the oropharynx
- O – Open: open the neonate’s mouth
- P – Pressure: If possible, increase the pressure being delivered. Initial pressure is 20 mmHg to 25 mmHg to 30 mmHg. This can be accomplished with a flow inflating bag or Neopuff.
- A – Alternate Airway: Consider intubation or supraglottic airway if weight permits.
- Continue down the PPV path until effective ventilation is maintained. Adjust the FiO2 to meet preductal target saturations (SpO2 probe must be on the right hand).
- If the HR remains in the 60-100 range with effective ventilation, then PPV must be maintained. If the HR increases to greater than 100 then PPV can be discontinued.
- If the HR drops to below 60 with effective ventilation, then chest compression must be initiated at a rate of 3 compressions to 1 ventilation. FiO2 should be at 100% at this point.
- If the HR remains below 60 EPINEPHrine should be administered. The dose is 10 mcg/kg.
- If there is a clinical history of blood loss and signs of poor perfusion a volume expander should be administered: either 10 ml/kg of normal saline or “O-negative“ PRBC.
- During the first 30 seconds, begin by assessing the neonate’s tone. Are they term, breathing or crying?
Additional Treatment Information
- Throughout a newborn resuscitation it is important to keep the neonate warm. Once a neonate becomes hypothermic, they become more susceptible to increased pulmonary vascular resistance; this in turn affects the oxygenation and ventilation of the neonate, and may reverse the transitioning back to fetal circulation, which is not compatible with life.
- EPINEPHrine can be administered via the endotracheal tube at a dose 10 times the IV dose - 100 mcg/kg.
- IV access can be via a peripheral IV or emergency UV
- IO can be considered but is weight dependent
- Uncuffed endotracheal tubes should be utilized to prevent the possibility of developing subglottic damage producing stenosis as the child grows
- All pre-term neonates of less than or equal to 32 weeks gestation should be placed in a food grade polyethylene bag up to the neck to prevent insensible fluid loss and maintain thermoneutrality
- A neonate delivered through thick meconium is at risk for developing increased work of breathing. If the child is vigorous, monitoring is suggested. If the neonate is not vigorous then suctioning of the oropharynx is required, followed by movement down the treatment path. The past practice of suctioning below the vocal cords is no longer recommended.
Referral Information
All neonates requiring resuscitation should be transported to hospital for further work up.
General Information
- ECG monitoring should be performed during the resuscitation.
- SpO2 monitoring must be via the pre-ductal right appendage for accurate measurements. A pre and post ductal (all other appendages) SpO2 can be monitored to detect the presence of shunts within the cardiovascular system.
- It is common for a neonate who experienced a precipitous delivery to develop increased work of breathing requiring respiratory support.
Interventions
Emergency Medical Responder (EMR) & All License Levels Interventions
- Ongoing care as dictated by NRP: follow algorithm
- Neonatal Resuscitation Algorithm
- Transport to the nearest hospital
- Seek additional resources or ACP intercept
Primary Care Paramedic (PCP) Interventions
- iGEL insertion if unable to oxygenate or ventilate
- Consider obtaining vascular access and providing fluid for hemodynamic compromise
- Correct hypoglycemia
Advanced Care Paramedic (ACP) Interventions
- Advanced airway intervention if unable to oxygenate or ventilate
- Obtain IO access if patient meets weight-based guidelines
- EPINEPHrine
Critical Care Paramedic (CCP) Interventions
- NIV/Invasive ventilation strategies
- Inotropic and vasopressors for hemodynamic instability
- Central Line and Arterial Line monitoring
- Blood product administration
- UV access (needs to be added as a schedule 2)
Algorithm