Confirmation
Pediatrics: Overview (For Consideration)
Updated:
Reviewed:
Introduction
For clinical consideration within BCEHS, pediatric patients are those who are ≤12 years of age, whereas adults are defined as >12 years of age or showing signs of puberty. There is widespread variation on this across Canada. This does not apply to matters of consent.
See BCEHS Pediatric Drug Dosages for age specific guidelines, vital signs and equipment sizes.
The Pedimate should be used during transport of pediatric patients between 10-40 lb (4.5-18 kg).
General Information
Pediatric Assessment
Children need to be treated differently from adults.
A child’s anatomy, physiology and response to illness and injury varies with age, and the spectrum of emergencies involving children is different to that of the adult population. Children’s vital signs, communication style, most likely diagnosis and treatment needs are age dependent, and many of their symptoms and all your equipment choices for diagnosis and care are size related. It is particularly important to always look for early signs of failure of respiratory, cardiovascular and nervous system function by assessing the work of breathing, circulation to the skin and appearance. The Pediatric Assessment Triangle (PAT) should be used to do this.
Pediatric Assessment Triangle
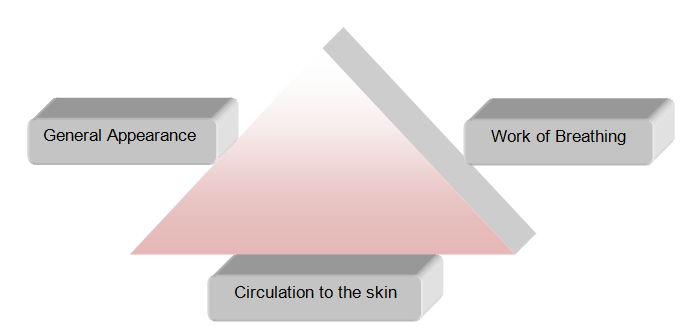
The PAT also enables the care giver to identify a child who is potentially unstable, and assess whether his/her condition is stable, improving or worsening over time. Clinical signs of progressive respiratory difficulty warn of impending respiratory arrest. In most instances in children, respiratory is the precipitating cause of cardiac arrest. Consequently, assessment and support of respiratory function is essential and the principal care entity and resuscitation measure required during pre-hospital care of infants and children.
Normal vital signs vary with age. Note that a younger child has a faster heart and respiratory rate and lower blood pressure. After about 12 years of age, normal vital signs approach adult values. Normal vital signs vary with age. Note that the younger the child, the faster the normal heart rate and the lower the normal blood pressure. After about 12 years of age, normal vital signs approach adult levels.
|
Age |
Weight (kg) |
Heart Rate (bpm) |
Respiratory Rate (bpm) |
Systolic BP (mmHg) |
|
Neonate |
< 3 |
100-160 |
40-60 |
Difficult to measure |
|
3 Months |
2 - 3 |
100-180 |
30-45 |
65-100 |
|
6 Months |
3 - 4 |
100-180 |
25-35 |
70-110 |
|
12 Months |
10 |
100-180 |
25-35 |
70-110 |
|
2 Years |
12 |
80-160 |
20-30 |
70-110 |
|
3-4 Years |
14-16 |
70-130 |
18-30 |
75-110 |
|
5-6 Years |
18-20 |
70-110 |
18-24 |
80-110 |
|
7-8 Years |
22-24 |
70-110 |
18-22 |
80-110 |
|
9-10 Years |
26-28 |
70-110 |
18-22 |
80-110 |
|
11-12 Years |
30-32 |
70-110 |
16-20 |
90-120 |
- Mean systolic BP can also be estimated by:
- 80 + (2 x Age) in years
- Lower limits of systolic BP can also be estimated by:
- 70 + (2 x Age) in years
- Weight can be approximated from the Broselow TM tape or:
- (Age (yr) x 2) + 8 = Wt (kg)
- Pounds/kilogram conversion:
- Wt (lb)/ 2.2 = Wt (kg)
Pediatric Respiratory Distress
Pediatric respiratory distress may look just like respiratory distress in adults, but may also present as:
- Rapid or slow respirations
- Nasal flaring
- Retractions
- Accessory muscle use
- Pale appearance
- Decreased breath sounds
- Mottled skin
- Grunting
- Stridor
- Wheezing
- Cyanosis
- Bradycardia
Pediatric Shock
Signs of shock or other serious illness may mimic those in adults, but may also include:
- Tachycardia/bradycardia
- Pale/cool/mottled skin
- Capillary refill>2 seconds
- Narrowing pulse pressure
- Tachypnea
- Relative flaccidity
- Change in level of consciousness (LOC) – especially failure to recognize / respond to parents
Pediatric Principles
Hypotension, a late and ominous sign of shock, means that cardio-respiratory arrest is imminent. A child may lose 25% of his/her circulating blood volume before becoming hypotensive. The signs and symptoms of shock listed above are much more sensitive than blood pressure.
A Broselow™ Pediatric Emergency tape is highly recommended as an aid to determining the patient’s weight and proper drug does and equipment sizes.
ET tube size can also be estimated by comparison to the size of the child’s nostril (nare), or the size of the child’s little finger, or by using the formula (age/4) + 4 = ET tube size. However, when a cuffed tube is to be used, calculate the tube size using the formula (age/4) +3. Children less than 1 year of age usually need a #1 straight laryngoscope blade, children 1-4 usually need a #2 blade and children >4 years usually need a #3 blade.
Abnormal Pediatric Vital Signs From the Pediatric Advanced Life Support Guidelines (PALS):
Hypotension is defined as follows:
|
For Term Neonates (0-28 days) |
SBP <60 mm Hg |
|
For Infants (1 month to 12 months) |
SBP <70 mm Hg |
|
For Children (>1 year to 10 years) |
SBP <70 + (2 x age in years) mm Hg |
|
For Adolescents (>10 years) |
SBP <90 mm Hg |
These figures overlap with the lower values for BP of 5% of the pediatric population who normally have low blood pressure. In assessing a child for the presence of shock it is important to consider the other clinical evidence such as a history suggestive of fluid or blood loss, sepsis, or major trauma, and clinical findings such as tachycardia, pallor cold extremities, altered mental state and increased work of breathing. Hypotension, especially with bradycardia, may signal impending arrest.