Confirmation
J02: Carbon Monoxide
Updated:
Reviewed:
Introduction
Carbon monoxide (CO) is a colourless, odourless, tasteless, non-irritating gas produced by the incomplete combustion of carbon-containing material such as gasoline, heating fuels, propane, oil, wood, and coal. Unintentional CO poisoning commonly results from inhalation of smoke from house fires, automobile exhaust, flue gas from furnaces or stoves, exhaust gas produced by outboard motors, ice-resurfacing machines, and barbecues used in poorly ventilated areas. Fatalities have been reported in those swimming near the engine exhaust outlets of boats, and where gas-powered stoves and generators are misused as an indoor heat source.
Natural gas and propane do not contain CO, but can produce CO if burned without enough air. Methylene chloride, a common ingredient in pain stripper, can be metabolized to carbon monoxide in the body after exposure.
Tobacco smokers have chronically elevated carboxyhemoglobin levels (see Toxic Dose).
Essentials
- Paramedics must contact CliniCall to speak with Paramedic Specialists regarding care planning for any suspected or confirmed carbon monoxide poisoning
- Remove patients to ambient air prior to assessment
- Decontamination is not required for patients exposed to carbon monoxide only. Patients who are removed from a house fire require a dry decontamination (i.e., removal of clothing) as a minimum measure before being loaded in an ambulance.
- High flow oxygen and supportive care is the treatment for all patients exposed to carbon monoxide
- ACP resources should be requested, if available, to measure COHb levels
- Fire departments can measure carbon monoxide levels inside buildings, and this should be accomplished where possible
- Standard pulse oximetry can be misleading in patients who have been exposed to carbon monoxide; these devices are only able to detect oxygenated and deoxygenated hemoglobin, and not any other form (such as carboxyhemoglobin or methemoglobin)
Additional Treatment Information
- Clinical Effects:
- An elevated carboxyhemoglobin (COHb) level is diagnostic of exposure, but may not reflect severity of poisoning or potential for development of delayed neurological sequelae. A more useful method of assessing the level of exposure may be to divide clinical signs into categories of severity. The category should be based on early symptoms.
- Mild: throbbing temporal headache, dizziness, nausea and vomiting, blurred vision
- Moderate: impaired thinking, confusion, severe headache, syncope or brief loss of consciousness, tachycardia, chest pain, dyspnea, tachypnea, and weakness
- Severe: myocardial ischemia, dysrhythmias, hypotension, cardiac arrest, respiratory failure, seizures, coma
Referral Information
Patients who have COHb levels between 3% and 10%, and who are symptomatic, require transport to hospital. Asymptomatic patients with COHb levels between 3% and 10% may not need transport, provided:
- The patient is with a responsible adult
- There is no history of ischemic heart disease
- The building is cleared of carbon monoxide
- The patient is not pregnant
- There is no history of syncope
Exposures above 10% require transport.
NB: these criteria depend on the ability to measure COHb, which is only available to ACP/CCP units in British Columbia. Point-of-care co-oximetry can be unreliable, and in-hospital arterial blood gas sampling can reveal significant discrepancies in the amount of COHb in a patient’s blood. Paramedics should, on the whole, be biased in favour of transporting patients with potential CO exposure to hospital for observation and additional evaluation.
General Information
- Carbon monoxide is readily absorbed after inhalation, and crosses the placenta. The elimination half-life of carbon monoxide is 4-5 hours breathing room air, 1-2 hours breathing 100% oxygen, and approximately 20 minutes with hyperbaric oxygen (2.5 atm).
- Hyperbaric oxygen (HBO) is a therapeutic option for treatment of CO poisoning. HBO produces a 10-fold increase in amount of oxygen dissolved in blood, increases oxygen delivery to hypoxic tissues, and enhances carbon monoxide elimination. HBO may also inhibit secondary cell damage (lipid peroxidation, mitochondrial dysfunction).
- Complications of HBO therapy are infrequent. Ear and sinus pain (common) are managed with decongestants and surgical myringotomy in a small number of patients. Confinement anxiety, pulmonary barotrauma, and oxygen toxicity seizures may occur rarely.
- Despite several prospective trials examining HBO in preventing delayed neurologic sequelae, it remains unclear which patients clearly benefit from HBO, or which clearly have no potential for benefit. Each patient must be assessed individually, evaluating potential benefits and risks. The following must be considered: current clinical status, time since exposure, acute vs chronic exposure, risk of transport, travel time to HBO chamber, concomitant diseases, and pregnancy status. Decision may be made in consultation with the poison control centre or the hyperbaric unit.
- Patients who may likely benefit from HBO treatment for CO poisoning include those with
- Neurologic signs: altered mental status, coma, cerebellar dysfunction, seizures
- History of loss of consciousness
- Pregnant patient with COHb level >20%
- Patients who may possibly benefit from HBO treatment for CO poisoning include those with
- Myocardial ischemia or cardiac dysrhythmias
- Metabolic acidosis
- Older patients
- Asymptomatic patients with COHb levels >25%
- Carbon monoxide poisoning can result in permanent neurologic damage and death. CO poisoning is one of leading causes of death worldwide; however, death is uncommon in patients who reach medical care. The major goal of treatment is prevention of delayed neurologic sequelae in survivors.
- The mechanism of toxicity is complex, and not fully understood. Toxicity is a result of hypoxia, ischemia, and direct cellular damage. CO binds to heme proteins, impairing normal oxygen function. Carbon monoxide-associated nitric oxide release may enhance oxidative and inflammatory injury to the brain. Carbon monoxide also has a direct effect on cellular respiration by inhibiting the activity of cytochrome oxidase and can provoke a metabolic acidosis.
- Hemoglobin has an affinity for carbon monoxide that is 200 to 250 times greater than its affinity for oxygen. Carboxyhemoglobin is formed, displacing oxygen from hemoglobin and producing a leftward shift in the oxyhemoglobin dissociation curve resulting in decreased oxygen delivery to tissues and hypoxia. Myoglobin is affected similarly, with its carbon monoxide affinity being 60 times greater. Impaired oxygen delivery may cause myocardial ischemia, resulting in dysrhythmias and systemic hypotension.
- The toxic dose of carbon monoxide is highly variable. The degree of poisoning is dependent on the concentration of carbon monoxide in the inspired air, the duration of exposure, the level of activity among those exposed, and the underlying health of patients. Infants, patients with pre-existing cardiovascular or lung disease, anemia, and in utero fetuses are more susceptible to carbon monoxide.
- Normal carboxyhemoglobin (COHb) blood levels in nonsmokers can be up to 2%. Smokers of 2-3 cigarette packages per day may have COHb levels up to 7-9%.
- Exposure to 545 ppm for 10 minutes has produced headache; inhalation of 5000 ppm for 5 minutes has been reported to be fatal.
- Automobile exhaust may contain up to 100,000 ppm (10%) carbon monoxide.
Interventions
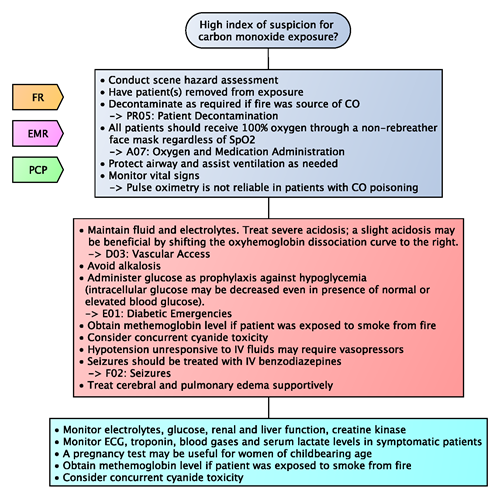
First Responder (FR) Interventions
- All patients should receive 100% oxygen through a non-rebreather face mask
Emergency Medical Responder (EMR) & All License Levels Interventions
- Conduct scene hazard assessment
- Have patient(s) removed from exposure
- Decontaminate as required if fire was source of CO
- In mild exposures, 100% oxygen should continue until patient is asymptomatic and carboxyhemoglobin (COHb) levels are < 5-6%
- To protect fetus, pregnant patients not receiving HBO may need to continue 100% oxygen 5 times longer than time required to reduce maternal COHb to < 5-6%
- In moderate and severely poisoned patients who are not candidates for hyperbaric oxygen, 100% oxygen may need to be continued for 24 hours after symptoms resolve
- Protect airway and assist ventilation as needed
- Monitor vital signs. Obtain carboxyhemoglobin (COHb) level to confirm exposure; results are not necessarily predictive of symptoms or outcome. Pulse oximetry is not reliable in patients with CO poisoning.
Advanced Care Paramedic (ACP) Interventions
- Maintain fluid and electrolytes. Treat severe acidosis; a slight acidosis may be beneficial by shifting the oxyhemoglobin dissociation curve to the right.
- Avoid alkalosis
- Administer glucose as prophylaxis against hypoglycemia (intracellular glucose may be decreased even in presence of normal or elevated blood glucose)
- Obtain methemoglobin level if patient was exposed to smoke from fire. Consider concurrent cyanide toxicity.
- Hypotension unresponsive to IV fluids may require vasopressors
- Seizures should be treated with IV benzodiazepines
- Treat cerebral and pulmonary edema supportively
Critical Care Paramedic (CCP) Interventions
- Monitor electrolytes, glucose, renal and liver function, creatine kinase
- Monitor ECG, troponin, blood gases and serum lactate levels in symptomatic patients. A pregnancy test may be useful for women of childbearing age.
- Obtain methemoglobin level if patient was exposed to smoke from fire. Consider concurrent cyanide toxicity.
Algorithm
Evidence Based Practice
References
- Alberta Health Services. AHS Medical Control Protocols: Carbon Monoxide Poisoning. 2020. [Link]