Confirmation
J05: Organophosphates and Carbamates
Updated:
Reviewed:
Introduction
Organophosphates and carbamates are groups of related chemicals commonly used as pesticides to control insects. Some preparations are approved for veterinary use to control fleas and other parasites. They are commonly formulated as dusts, granules, emulsions, suspensions, or solutions. Concentrates are often formulated in a petroleum distillate base.
Clinically, poisonings from organophosphates and carbamates are similar to each other, and results from the inhibition of acetylcholinesterase and the stimulation of muscarinic and nicotinic receptors. Carbamate toxicity is generally of shorter duration, as its effect on acetylcholinesterase is reversible.
Deaths from these products occur as a result of acute respiratory failure.
Essentials
- Paramedics must contact CliniCall (1-833-829-4099) to discuss the case, ideally prior to arrival at scene
- Decontamination requirements can be complex and must be completed prior to moving the patient to the ambulance for treatment.
- Attempt to identify the name and amount of the substance the patient was exposed to, including the pesticide control number, WHMIS information, or photo of the label. This can be sent to CliniCall for additional information.
- Health care staff, including paramedics, should wear protective clothing when handling contaminated clothing and grossly contaminated patients.
- Treatment should be directed at decontamination, administration of antidotes where available, and support for oxygenation and ventilation.
Additional Treatment Information
- Activated charcoal may be considered in hospital for up to one hour post-ingestion
- High doses of atropine, in conjunction with pralidoxime, may be required in cases of severe organophosphate poisoning
General Information
- Organophosphate pesticides include: acephate, azinphos-methyl, chlorpyrifos, diazinon, dichlorvos, dimethoate, fenthion, malathion, methamidophos, naled, phorate, propetamphos, terbufos, tetrachlorvinphos, trichlorfon.
- Carbamates include: bendiocarb, carbaryl, carbofuran, formetanate, methomyl, oxamyl, propoxur.
- Products may be labeled as “systemic” or “contact” – this refers to the action of the pesticide and whether it is taken into plant tissues. It has no bearing on human toxicity.
- The onset of symptoms is usually within minutes to hours after exposure. Symptoms may be delayed in the case of skin exposure.
- Symptoms can be divided into muscarinic effects – miosis, excessive sweating and bronchial secretions, bradycardia, hypotension – and nicotinic effects (mydriasis, tachycardia, fasiculations, muscle weakness and paralysis). Central nervous system effects can include headache, drowsiness, seizures, and unconsciousness.
- Muscarinic receptors are predominantely in the parasympathetic nervous system, whereas nicotinic receptors are primarily in the sympathetic nervous system.
- A useful mnemonic for organophosphate toxicity is SLUDGEM/BBB:
- Salivation
- Lacrimation
- Urination
- Defecation
- GI upset
- Emesis
- Miosis
- Bronchorrhea
- Bronchospasm
- Bradycardia
- The three “Bs” – bronchorrhea, bronchospasm, and bradycardia – are the most common causes of death in organophosphate and carbamate poisoning.
Interventions
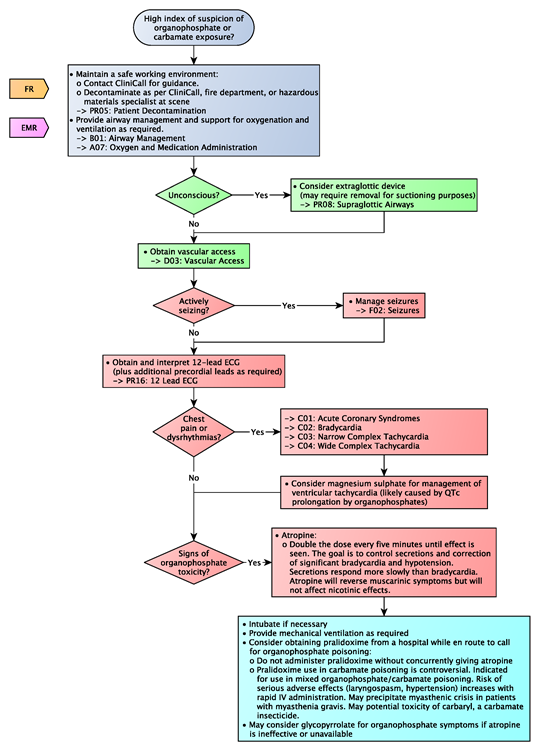
First Responder (FR) Interventions
- Maintain a safe working environment:
- Contact CliniCall for guidance
- Decontaminate as per CliniCall, fire department, or hazardous materials specialist at scene
- Provide airway management and support for oxygenation and ventilation as required
Primary Care Paramedic (PCP) Interventions
- Consider extraglottic device for profoundly unconscious patients (may require removal for suctioning purposes)
- Obtain vascular access
Advanced Care Paramedic (ACP) Interventions
- Manage seizures
- Treat dysrhythmia and chest discomfort as per CPGs
- Consider magnesium sulfate for management of ventricular tachycardia (likely caused by QTc prolongation by organophosphates)
- Atropine:
- Double the dose every five minutes until effect is seen. The goal is to control secretions and correction of significant bradycardia and hypotension. Secretions respond more slowly than bradycardia. Atropine will reverse muscarinic symptoms but will not affect nicotinic effects.
Critical Care Paramedic (CCP) Interventions
- Intubate if necessary
- Provide mechanical ventilation as required
- Consider obtaining pralidoxime from a hospital while en route to call for organophosphate poisoning:
- Do not administer pralidoxime without concurrently giving atropine
- Adults:
- Loading dose: 1 – 2 g IV infused over 30 minutes. May be given by direct IV injection over 5 minutes in severely poisoned patients. First dose may be given IM if IV access is not possible.
- Maintenance dose: continuous infusions preferred. Optimal dose not established; 500 mg/hr is often recommended. Consider 8-10 mg/kg/hr (as per WHO guidance). Lower rates may be adequate. Titrate to response.
- Children:
- Loading dose: 20-50 mg/kg. May also be given by direct IV injection over 5 minutes, or IM if IV access cannot be obtained.
- Maintenance dose: 10-20 mg/kg/hr.
- Therapeutic endpoint: control of nicotinic symptoms. Treatment for 24-48 hours is usually sufficient in many cases. Prolonged treatment (i.e., several weeks) may be required in severe poisoning. Discontinue when patients no longer require ventilatory support.
- Adults:
- Pralidoxime use in carbamate poisoning is controversial. Indicated for use in mixed organophosphate/carbamate poisoning. Risk of serious adverse effects (laryngospasm, hypertension) increases with rapid IV administration. May precipitate myasthenic crisis in patients with myasthenia gravis. May potential toxicity of carbaryl, a carbamate insecticide.
- Do not administer pralidoxime without concurrently giving atropine
- May consider glycopyrrolate for organophosphate symptoms if atropine is ineffective or unavailable
Algorithm